


MPHI provides staffing and technical assistance to two cancer-screening programs that are funded by the Centers for Disease Control and Prevention (CDC), Michigan’s “Breast and Cervical Cancer Screening Program” and the “Colorectal Cancer Early Detection Program.” These programs use comprehensive protocols to help ensure high-quality clinical services and data-tracking methodologies, including reimbursement monitoring. MPHI conducts data reporting and analysis, financial management, billing, and reimbursement.
From 1991-2015, more than 10,000 women were diagnosed with breast or cervical cancer (or cervical pre-cancerous lesions) through this program, which utilizes the services of a network of 19 coordinating agencies covering all 83 of Michigan’s counties. Since 2002, women enrolled in the program who were diagnosed with breast or cervical cancer automatically became eligible to apply for Medicaid to cover all treatment needs.
This program has provided screening and follow-up services to approximately 25,500 low-income women in Michigan each year since 1991, until the Healthy Michigan Plan began enrolling clients in April 2014. The program now enrolls approximately 9,000 women per year.
The colorectal program began in 2011 and operates on a model similar to the Breast and Cervical Cancer Screening Program. It provides screening and diagnostic testing to approximately 700 low-income people aged 50-64 each year.
Since its inception, the program has provided more than 4,500 screenings, found 228 cases of precancerous adenomatous polyps, and diagnosed five colorectal cancers.
The Michigan Breast and Cervical Information System (MBCIS) serves as the centralized database for both programs, and houses information critical to managing quality and facilitating reporting mechanisms to local agencies and the CDC. The system also processes medical claims according to program protocols. The MBCIS is housed on State of Michigan servers.
MPHI has helped both cancer-screening programs maintain high standards of clinical service delivery and data management for 17 years by overseeing data management, quality improvement, and evaluation efforts. More information about these programs can be found at http://www.michigancancer.org/BCCCP/ or http://www.michigancancer.org/colorectal/.

In February 2015, the Robert Wood Johnson Foundation (RWJF) selected MPHI, in partnership with the Illinois Public Health Institute (IPHI), to serve as the National Coordinating Office for a new initiative to foster multi-sector information systems to improve community health.
Connections among public health, health care, human services, and other sectors can improve communities’ capacity for planning, prioritizing, monitoring, innovation, and rapid response for healthier and more resilient populations. “Data Across Sectors for Health” (DASH) aims to identify and share learnings to move the field toward action.
In the first year, MPHI conducted an environmental scan to identify barriers, opportunities, promising practices, and indicators of progress for multi-sector collaborations to connect information systems and share data for community health improvement. MPHI also supported IPHI in fielding a $2 million call for proposals (CFP) that generated more than 400 responses.
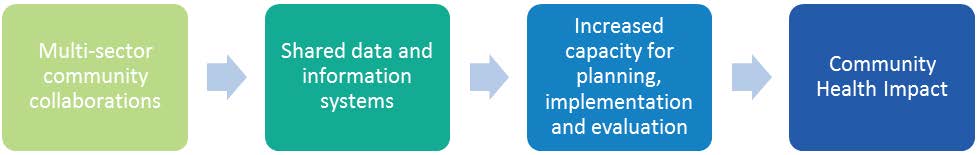
The ten awarded 12-18 month grants will help test a theory of change. Increases along any of three domains ̶̶ data sharing and connected information systems, the degree and nature of collaboration, or the number of sectors ̶̶ will increase community capacity for taking action. These increases lead to improvements in community health.
The excitement generated by the CFP led RWJF to reconsider the importance of DASH in their work toward building a culture of health across the nation. Going into year 2, DASH is a National Program Office with 10 grantees and the following tasks.
These activities will have the following impact.

Nearly every baby born in the U.S. is tested shortly after birth for inborn errors of metabolism (IBEM) through newborn blood spot screening (NBS). This screening identifies rare and life-threatening conditions to save lives and protect children from developing preventable disabilities. After more than 50 years of NBS, however, few of the conditions have an evidence base to guide their management and enable people to develop their full potential for healthy and productive lives.
The “Inborn Errors of Metabolism Collaborative” (IBEMC) originated in 2005 when seven clinicians came together to collect data to provide long-term follow-up for patients with rare IBEM. From 2005-2010, the Region 4 Genetics Collaborative supported this group. Region 4 is housed at and managed by MPHI, and is funded by the federal Health Resources and Services Administration (HRSA). Region 4 brought together clinicians and public health partners to provide input into data elements to be included in the Inborn Errors of Metabolism Information System (IBEM-IS). This resulted in a data set that enhances knowledge of clinical outcomes and supports public health surveillance and policy development. Collaborators defined condition-specific elements for the metabolic conditions identified on the recommended uniform screening panel. The IBEM-IS was ultimately adopted for national use; it provides the foundation for collecting the information required for long-term follow-up in IBEM.
In 2011, the National Institute for Child Health and Human Development awarded the IBEMC a five-year grant to study the natural history of IBEM. This funding supported data collection from 13 clinics to improve scientific knowledge about the natural history of IBEM and gather evidence of effective management and treatment strategies.
As the IBEMC gained recognition, other HRSA-funded Regional Genetics Collaboratives supported additional clinics to contribute. These extended partnerships have resulted in the largest single collection of clinical information about newborn-screened conditions, including data on more than 1,800 patients entered by 27 clinics in 19 states.
In August 2014, the IBEMC convened 30 clinicians and researchers to identify concerns facing NBS and the management of IBEM. They prioritized the following issues as most important to the identification and treatment of individuals with IBEM.
To address these issues, MPHI applied for additional funds from the National Institutes of Health in 2015 for the “Long-Term Follow-Up to Develop Evidence-Based Newborn Screening and Management Strategies for Inborn Errors of Metabolism” project. The goal of the program is to provide evidence-based recommendations for care management that will support individuals with IBEM to reach their full potential for healthy, productive lives. If funding is received, this program will begin in September 2016 with the following aims.

The “Michigan Care Improvement Registry” (MCIR) tracks Michigan residents’ vaccine histories and makes the information available to immunization providers, schools, and child care centers in the state. From MCIR’s inception, MPHI has assisted the Michigan Department of Health and Human Services with the registry’s development and implementation.
Prior to the creation of MCIR in 1997, the immunization histories of children who received vaccines at a variety of locations were not centrally tracked, and many children received duplicate doses of vaccines because of incomplete records. MCIR provides a centralized repository for vaccination data and includes a forecasting feature that provides information about when another dose is due.
Immunization providers are required by the public health code to enter the vaccines administered to children under 20 years old into the registry. Although they are not required by law to enter adult data, most enter the immunizations they administer to people of all ages.
Today, MPHI provides technical and programmatic assistance to continue developing, deploying, and supporting statewide use of the registry by Michigan’s immunization providers, schools, and child care centers. Services include data quality management, technological support, technical assistance, information dissemination, electronic submission approval, website management, project planning, and management services.
Visit www.mcir.org for more information.

In 2005, with funds from the federal Health Resources and Services Administration’s Maternal and Child Health Bureau, MPHI launched the “National Child Death Review Case Reporting System” (CRS). CRS is a database of comprehensive information on the circumstances of individual child deaths that are reviewed by local and state Child Death Review teams in 44 participating states. The database currently contains information on the deaths of more than 157,000 children.
MPHI’s National Center for the Review & Prevention of Child Deaths allows researchers to access the data through a formal application process. Recent papers using the data include an article on mortality and epilepsy in Epilepsy & Behavior and one on pediatric suicide, which was submitted to Injury Prevention.
Researchers are currently analyzing data on child maltreatment with the National Center for Health Statistics and on infant death in sleep with the Children’s National Medical Center.
Visit www.childdeathreview.org for additional information.